Hypoglycemia, or low blood sugar, is often associated with diabetes management. While most people think of diabetes as a condition characterized by high blood sugar (hyperglycemia), it’s also possible for individuals with diabetes to experience hypoglycemia. This article explores why can diabetes experience hypoglycemia, the symptoms to watch for, and how to manage and prevent episodes effectively.
What Is Hypoglycemia?
Hypoglycemia occurs when blood sugar levels drop below 70 mg/dL, although individual thresholds may vary. It’s a condition that can cause a range of symptoms, from mild discomfort to severe complications if left untreated. For people with diabetes, hypoglycemia is often a result of their treatment regimen, such as the use of insulin or other blood sugar-lowering medications.
Read too: What is Diabetic Profile Test? A Complete Guide to Understanding Its Importance and Procedure
Can Diabetes Experience Hypoglycemia?
Yes, individuals with diabetes can experience hypoglycemia, particularly those managing their condition with insulin or medications that increase insulin production. Here’s why it happens:
1. Excessive Insulin
When too much insulin is administered, it can lower blood sugar levels more than intended. This is a common cause of hypoglycemia in individuals using insulin therapy.
2. Skipping Meals
Skipping or delaying meals can cause blood sugar levels to drop, especially if diabetes medications are taken without enough food.
3. Increased Physical Activity
Exercise increases glucose utilization by the muscles, which can lead to hypoglycemia if meals or snacks aren’t adjusted accordingly.
4. Alcohol Consumption
Drinking alcohol on an empty stomach can interfere with the liver’s ability to release glucose into the bloodstream, increasing the risk of low blood sugar.
5. Medication Errors
Taking the wrong dose of medication or combining diabetes drugs with other treatments can lead to hypoglycemia.
6. Other Health Conditions
Illnesses like kidney or liver disease can affect blood sugar regulation, making hypoglycemia more likely.
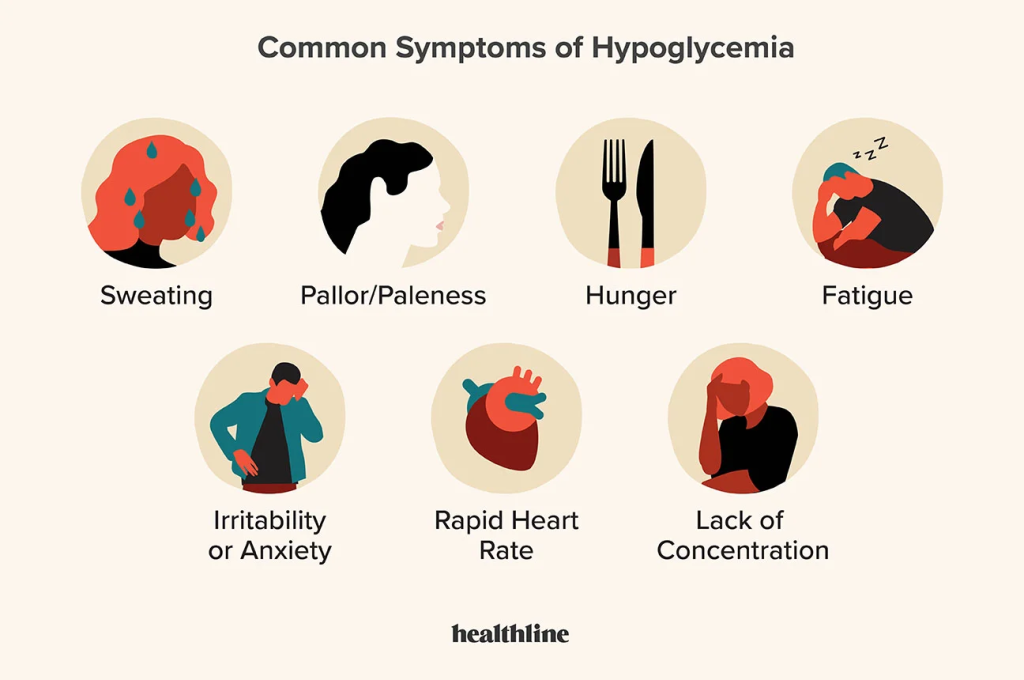
Symptoms of Hypoglycemia in Diabetes
Recognizing the symptoms of hypoglycemia is crucial for prompt treatment. Common symptoms include:
- Shaking or trembling.
- Sweating.
- Dizziness or lightheadedness.
- Rapid heartbeat.
- Hunger.
- Irritability or mood changes.
- Confusion or difficulty concentrating.
In severe cases, hypoglycemia can lead to:
- Loss of consciousness.
- Seizures.
- Coma.
If you or someone you know with diabetes experiences severe symptoms, it’s essential to seek medical help immediately.
Why Can Diabetes Experience Hypoglycemia More Frequently?
Diabetes treatments aim to maintain blood sugar levels within a target range. However, achieving tight control increases the risk of hypoglycemia. Factors that make hypoglycemia more frequent in diabetes include:
- Intensive Insulin Therapy: Individuals with type 1 diabetes or advanced type 2 diabetes often require multiple daily insulin injections or insulin pumps, which can increase the risk of errors or fluctuations.
- Long-Term Diabetes: Over time, the body’s ability to signal low blood sugar may diminish, a condition known as hypoglycemia unawareness.
- Combination Medications: Certain oral medications combined with insulin therapy can heighten the likelihood of hypoglycemia.
How Can Diabetes Experience Hypoglycemia Be Prevented?
Preventing hypoglycemia involves a proactive approach to blood sugar management. Here are key strategies:
1. Monitor Blood Sugar Regularly
Frequent blood sugar checks allow individuals to identify patterns and take corrective actions before hypoglycemia occurs.
2. Follow a Consistent Meal Schedule
Eating balanced meals and snacks at regular intervals can help stabilize blood sugar levels. Include complex carbohydrates, lean proteins, and healthy fats in your diet.
3. Adjust Medications as Needed
Work with your healthcare provider to fine-tune your medication doses based on your activity levels, meal plans, and other factors.
4. Plan for Exercise
Always check your blood sugar before, during, and after physical activity. Carry snacks or glucose tablets to prevent exercise-induced hypoglycemia.
5. Limit Alcohol
Avoid drinking on an empty stomach and monitor blood sugar levels closely if you consume alcohol.
6. Be Prepared
Carry fast-acting glucose sources, such as glucose tablets, candy, or juice, to treat hypoglycemia quickly.
Managing Hypoglycemia in Diabetes
If you experience symptoms of low blood sugar, it’s essential to act quickly to prevent the situation from worsening. Here’s what to do:
1. The 15-15 Rule
Consume 15 grams of fast-acting carbohydrates (e.g., 4 glucose tablets, a small glass of juice, or regular soda). Wait 15 minutes and check your blood sugar. If it’s still low, repeat.
2. Long-Term Glucose Source
Once your blood sugar is back to normal, eat a snack or meal containing protein and complex carbohydrates to maintain stability.
3. Educate Your Support Network
Ensure family, friends, and coworkers know how to recognize hypoglycemia and assist you during an episode.
4. Use Glucagon for Severe Cases
If you’re unable to treat hypoglycemia yourself, someone else can administer glucagon, a hormone that raises blood sugar levels. Speak with your healthcare provider about keeping a glucagon emergency kit on hand.
How Does Hypoglycemia Differ by Diabetes Type?
While both type 1 and type 2 diabetes patients can experience hypoglycemia, the underlying causes and risk factors may differ:
Type 1 Diabetes
- Greater reliance on insulin therapy increases the risk of low blood sugar.
- Hypoglycemia unawareness is more common due to repeated episodes over time.
Type 2 Diabetes
- Some medications, like sulfonylureas, increase the risk of hypoglycemia.
- Patients managing diabetes with diet and exercise alone are less likely to experience hypoglycemia.
When to Seek Medical Help
While mild hypoglycemia can often be managed at home, severe episodes require medical intervention. Seek help if:
- You lose consciousness.
- You experience recurrent or severe hypoglycemia despite preventive efforts.
- Your blood sugar does not stabilize after treatment.
Living with Diabetes: Balancing the Risks of Hypoglycemia
Managing diabetes is a balancing act between preventing hyperglycemia and avoiding hypoglycemia. By staying informed and proactive, individuals can reduce the frequency and severity of hypoglycemic episodes.
Support from Healthcare Providers
Regular check-ins with your diabetes care team can help address concerns, adjust treatments, and provide personalized advice for managing hypoglycemia.
Community Resources
Connecting with others who share similar experiences can offer emotional support and practical tips. Online forums, local diabetes support groups, and educational workshops are valuable resources.
Conclusion
Can diabetes experience hypoglycemia? Absolutely. Understanding the causes, symptoms, and management strategies for hypoglycemia is essential for anyone living with diabetes. By staying vigilant and adopting preventive measures, individuals can reduce the risk of low blood sugar and maintain better overall health. Always consult your healthcare provider to develop a management plan tailored to your needs.

Leave a Reply